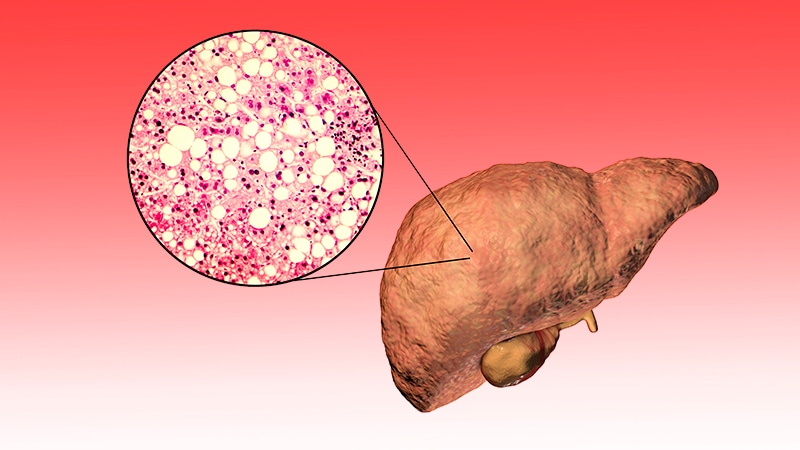
More than 30% of people worldwide have metabolic dysfunction–associated steatotic liver disease (MASLD; formerly nonalcoholic fatty liver disease), including 65% of those with type 2 diabetes (T2D) and 75% of those with obesity.
At the “Innere Medizin fachübergreifend — Diabetologie grenzenlos” congress held on February 7 and 8 in Munich, Germany, Martina Müller-Schilling, MD, MHBA, chair and director of the Department of Internal Medicine I at University Hospital Regensburg, Regensburg, Germany, explained that the rising prevalence of MASLD is linked to the “obesity pandemic” in industrialized nations.
MASLD is a steatotic liver disease associated with at least one cardiometabolic risk factor unrelated to alcohol consumption and is particularly common in individuals with T2D. Due to improved diabetes treatments, patients are now experiencing “new complications from a decade-long chronic and systemic disease,” Müller-Schilling noted.
The updated nomenclature for MASLD and metabolic dysfunction–associated steatohepatitis (MASH; formerly nonalcoholic steatohepatitis), expected in mid-2024, aims to highlight the metabolic nature of the disease and reduce the stigma associated with alcohol-related liver conditions.
Screening Criteria
A targeted case-finding approach is recommended for screening at-risk individuals, including:
- Patients with unexplained elevated liver enzymes (eg, without viral hepatitis)
- Individuals with obesity and hypertension
- Adults with T2D
According to Müller-Schilling, MASLD is often detected incidentally in a general practitioner’s office. For example, if a patient has symptoms suggesting gallstones, it could also be steatotic liver disease or fatty liver disease.
In primary care, initial screening can include ultrasound and testing of liver enzyme levels.
Additionally, if cardiovascular risk factors and comorbidities, such as T2D, hypertension, or obesity, are present along with abnormal liver enzymes or imaging signs of hepatic steatosis, further assessment with the Fibrosis-4 blood test and enhanced liver fibrosis test can help determine fibrosis severity.
Further assessment of fibrosis stage and risk stratification should be conducted in a specialist outpatient clinic. “Fibrosis is a precancerous condition,” said Müller-Schilling, and “the most common indication for a liver transplant in the next 10 years.” However, she emphasized that prevention is possible through awareness. Early diagnosis, intervention, and appropriate management can prevent progression to cirrhosis.
Prevention and Diagnostic Strategies
Imaging and blood tests allow for risk stratification of liver-related complications and mortality, making them useful for monitoring disease progression, Müller-Schilling said.
To assess the severity of fibrosis, biomarker scores are used with elastography, which measures liver stiffness. However, the key microscopic features of MASLD, such as ballooning or lobular inflammation, can only be identified histologically through liver biopsy.
A recent study published in Cell Metabolism, which Müller-Schilling presented, evaluated a blood test for MASLD/MASH in 700 participants from the United States and China. The researchers used a three-parameter (N3) biomarker panel, which included chemokine ligand CXCL10, cytokeratin 18 fragment M30, and an adjusted body mass index.
The test effectively distinguished healthy individuals from those with MASLD. It could also identify patients with MASH among those with MASLD with a specificity of 90%, a sensitivity of 62.9%, and a positive predictive value of 88.6%.
The study also showed that the test could detect MASH improvement over time.
The authors wrote that they “developed a robust blood-based panel for the noninvasive diagnosis of MASH, which might help clinicians reduce unnecessary liver biopsies.”
Lifestyle Changes
For patients with F0/F1 fibrosis, lifestyle interventions are the first-line treatment, explained Andreas Geier, MD, from the Division of Hepatology, University Hospital Würzburg, Würzburg, Germany.
Studies have shown that reducing caloric intake by 500 kcal/d can improve fibrosis; however, weight loss often leads to a rebound, even with glucagon-like peptide 1 (GLP-1) receptor antagonists, as fibrosis tends to worsen when patients regain weight.
Exercise
A 2024 study suggested that exercise may be more effective than weight loss alone. The study evaluated a calorie-restricted diet combined with 4 × 4–minute exercise intervals (three times/wk for 10 months) and found significant improvements in MASH compared with the standard treatment.
After 10 months, patients in the intervention group had greater reductions in body weight, body fat, and liver damage than those who received standard treatment. Additionally, peak oxygen consumption and peripheral insulin resistance, both linked to MASH, also improved.
Geier noted that this study had a small sample size of 24 patients. However, he emphasized the “scientific rationale for exercise as a behavioral intervention for effective and significant liver fat reduction,” which is why the current guidelines recommend a combination of diet and exercise.
Treatment
In addition to lifestyle changes, GLP-1 receptor agonists, such as semaglutide, are now part of clinical obesity management, as explained by Müller-Schilling. Comorbidities can also be managed with medication, including:
- T2D treated with GLP-1 receptor agonists, coagonists, sodium-glucose cotransporter-2 inhibitors, metformin, or insulin (for decompensated cirrhosis)
- Dyslipidemia managed with statins
- Obesity with GLP-1 receptor agonists and coagonists as well as bariatric interventions
Resmetirom, a thyroid hormone receptor beta agonist, became the first drug approved for MASH in the United States in early 2024. Real-world data suggest promising benefits for patients; however, approval from the European Medicines Agency for use in the European Union is still pending.
Müller-Schilling emphasized the need for targeted therapies for MASLD/MASH. She highlighted the role of biomarkers in assessing treatment response and categorizing patients, similar to the approaches used in oncology and gastroenterology.
This story was translated from Medscape’s German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Source link : https://www.medscape.com/viewarticle/growing-burden-fatty-liver-disease-whats-next-2025a10004vz?src=rss
Author :
Publish date : 2025-02-26 10:17:54
Copyright for syndicated content belongs to the linked Source.