[ad_1]
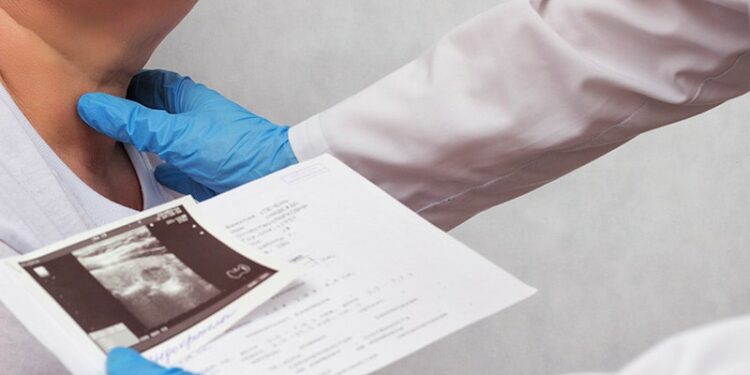
The incidence of thyroid cancer in the United States, having plateaued in 2009 after a decades-long increase, has remained stable since then, despite efforts to control an ongoing overdiagnosis of the disease, new research shows.
“Although the incidence of thyroid cancer has plateaued, it remains at peak levels, suggesting that overdiagnosis remains a crucial unresolved public health issue,” reported the authors of the study, published this month in the Lancet Diabetes & Endocrinology.
“If these trends persist, there will be a long-term persistence in a vast number of thyroid cancer cases that have been overdiagnosed, representing an area of utmost public health concern,” they added.
The findings are from a retrospective study of data on 91,968 patients with thyroid cancer identified in the National Cancer Institute’s Surveillance, Epidemiology, and End Results database and the National Center for Health Statistics database, spanning the time frame from 1975 to 2019.
The data showed the annual incidence of thyroid cancer in the United States increased from 5.0 cases per 100,000 people in 1975 to 14.6 cases per 100,000 people in 2009.
Afterwards, however, the incidence rate plateaued and remained stable until the end of the study period in 2019.
Importantly, rates of thyroid cancer mortality and metastasis at diagnosis over the study period remained relatively stable.
The sharp increase of detections prior to the plateau appears to have corresponded with changes in clinical practice, most notably the increased use of medical imaging, “leading to the increased detection of thyroid nodules and subsequent diagnoses of thyroid cancer,” the authors noted.
The increase in incidence was most prominent among women aged 40-69 years and men aged 50-79 years, further supporting the conclusion that the increase represents overdiagnosis, since those age groups are most likely to have higher interaction with health care, hence an increased likelihood of imaging detecting an incidental thyroid nodule.
“Collectively, these data strongly suggest that both the age-specific and sex-specific variations seen in the incidence of thyroid cancer in current clinical practice are primarily driven by period-dependent increases in the overdiagnosis of clinically indolent thyroid cancers,” the authors wrote.
Greater Response Was Expected After Guideline Changes
With a large series from 2008 showing that the vast majority of papillary thyroid microcarcinomas (over 99%) are not at risk for distant metastases,the American Thyroid Association changed its management guidelines for thyroid nodules the next year, in 2009, detailing new recommendations against the biopsy of most small, low-risk thyroid nodules.
Subsequently, practice guidelines to prevent overdiagnoses were also adopted by the Endocrine Society in its Choosing Wisely guidelines in 2013 and again in 2017 and 2018, which recommended against routine thyroid ultrasonography in patients with atypical thyroid function test results in the absence of any palpable abnormality.
Likewise, the US Preventive Services Task Force also changed its recommendations in 2017.
However, while some studies have suggested a decline in the incidence since those developments, the current study shows no similar trends.
“Thyroid cancer incidence rates are frozen at peak levels,” first author Zachary S. Zumsteg, MD, an associate professor of the Department of Radiation Oncology, at Samuel Oschin Comprehensive Cancer Institute, Cedars-Sinai Medical Center, Los Angeles, told Medscape Medical News.
“There is much more that needs to be done to address this problem.”
Key changes the authors called for include “novel imaging strategies to better identify thyroid nodules that require biopsy, along with advancements in molecular testing to decrease the rate of indeterminate thyroid biopsies.”
Harms of Overdiagnosis; More Work Needed
Zumsteg underscores that overdiagnosis can pose risks of its own to patients, including economic costs, potentially unnecessary invasive procedures, and significant psychological harms relating to worry about the cancer.
“I think we all wanted to believe that with increasing recognition of the harm that thyroid imaging in asymptomatic patients can pose, supported by multiple well-respected guidelines, that we would be able to reduce thyroid cancer overdiagnosis,” Zumsteg said.
“We have made progress in some ways, as the rapid year-over-year increase overdiagnosis has been stopped,” he added. “However, we seem to be stuck at essentially peak overdiagnosis levels.”
“There may have been a slight decline over the past decade or so, but it is so small that it was not detectable statistically in our study. This means we have a lot of work to do.”
The issue of papillary microcarcinomas being detected in asymptomatic patients receiving imaging for other purposes is an especially tricky challenge, since that imaging is typically necessary — as is the need for the highly precise imaging that may wind up detecting the incidental thyroid nodules, Zumsteg said.
“If a patient receives imaging for a completely unrelated issues and is found to have a thyroid nodule, this is difficult to prevent,” he said.
To address the challenge, Zumsteg called for a multipronged approach.
“First, we need better research regarding which of these nodules need any work-up at all,” he said. “Second, we need to continue to understand how to best distinguish life-threatening thyroid cancers from those with virtually no mortality risk on a molecular level.”
“Last, understanding that complete elimination of asymptomatic thyroid nodules and indolent thyroid cancer is not possible, the thyroid cancer community need to embrace active surveillance approaches,” Zumsteg added.
“This has been very successfully implemented for low-risk prostate cancer, where it is the preferred strategy,” he noted.
“Even if we can’t completely eliminate overdiagnosis, we should be able to significantly limit overtreatment.”
Trend Seen Beyond the United States
Findings from another study, published in November 2024, also in Lancet Diabetes & Endocrinology also details that the extent of thyroid cancer overdiagnosis is seen well beyond the United States.
In the study covering 63 countries across five continents, overall, 75.6% of thyroid cancer cases were attributable to overdiagnosis, with the highest rates (85%) occurring in in Cyprus, China, South Korea, and Turkey.
“Although the incidence of thyroid cancer has reached a plateau or decrease in some high-income countries, the magnitude of overdiagnosis is still very large and the expansion of overdiagnosis of thyroid cancer to the transitioning countries has been rapid, which makes it a global public health challenge that needs to be addressed,” the authors of that study concluded.
The authors had no significant disclosures to report.
[ad_2]
Source link : https://www.medscape.com/viewarticle/thyroid-cancer-rates-remain-frozen-amid-overdiagnosis-2025a10003ve?src=rss
Author :
Publish date : 2025-02-14 09:17:14
Copyright for syndicated content belongs to the linked Source.